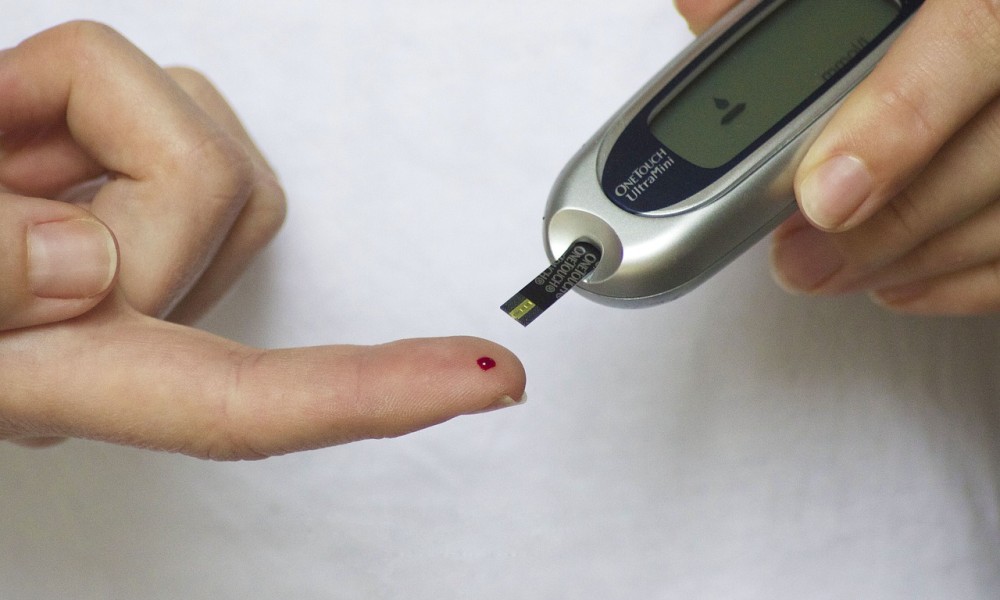
An Indian American scientist Sanjay Basu from Stanford University and his team has found that widespread diabetes screening in India is ineffective and glucometer-based screening tools are unlikely to meet effectiveness criteria.
For the new study, the researchers developed a micro-simulation model – a computer model that operates at the level of individuals – to investigate the implications of using alternative screening instruments to identify people with undetected diabetes across India.
They found out that:
- Between 158 million and 306 million of the 567 million Indians eligible for screening would be referred for confirmatory testing, depending on which approach was used for screening.
- Between 126million and 273 million of these high-risk individuals would be false positives
- Only between 26 million and 37 million would meet the international diagnostic criteria for diabetes
- The ratio of false positives to true positives varied from 3.9 (when using random glucose screening) to 8.2 (when using a survey-based screening instrument) in this model.
The researchers estimate that the cost per case found would vary from $5.28 (Rs.336) for random glucose screening) to $17.06 (Rs.1087) for a survey-based screening instrument. They also estimate that the total cost for screening the eligible population would be around $169 – $567 million.
Limitations of this study include the uncertainty of modelling a large, diverse population and of forecasting costs. But, the findings of poor test specificity are consistent with results from small, regional trials in India.
The authors of the study suggest,
[whatsapp]
“Focusing on symptom-based screening and on improvements to diabetes treatment might better serve India’s population.”
Sanjay Basu’s award of $100,000, George Rosenkranz Prize for Health Care Research in Developing Countries in 2014, has helped fund this large-scale data collection project in India to improve Type-2 diabetes screening in the country, leading to better treatment and detection of the disease.
The study has been published in the journal PLOS Medicine.

