
Long COVID: This Is Why Some Patients Who Have Recovered From COVID-19 Still Aren’t Well
COVID-19 is changing colours faster than a chameleon as it continues to attack the human body in diverse ways. While most people recover from Covid-19 in a matter of weeks, there is a growing body of evidence that it may be a long-term condition for some.
As the number of patients, who are left experiencing symptoms months after being infected is on an exponential rise, scientists and doctors, across the globe are now beginning to urge the global community to focus on something called long COVID and even the World Health Organization (WHO) is beginning to take note and initiate public health action against it.
So, what is long COVID and why do you need to know about it urgently?
What is long COVID?
There is no medical definition or list of symptoms shared by all patients – two people with long COVID can have very different experiences. However, patients who recovered early on are now noting that their symptoms often last for months on end despite the infection itself abating quickly.
This suggests that these patients are not actually recovering from COVID-19 and may have other complications or morbidities too. This long-term experience of debilitating symptoms is being referred to as long COVID. The people it affects — who sometimes call themselves “long-haulers” — experience either flare-ups or continuous symptoms of illness.
What are the symptoms of long COVID?
The most common and discussed feature of long COVID is crippling fatigue. As the most commonly reported symptom that persists for months, fatigue can affect everything from your physical health to mental health. A recent article published in Nature recommends that comparison of fatigue due to long COVID and chronic fatigue syndrome is needed to better understand this condition.
Similarly, a high frequency of COVID-19 patients has been observed to be suffering from post-viral or inflammatory myocarditis, which not only leads to sustained arrhythmias but also to heart failure in the future.
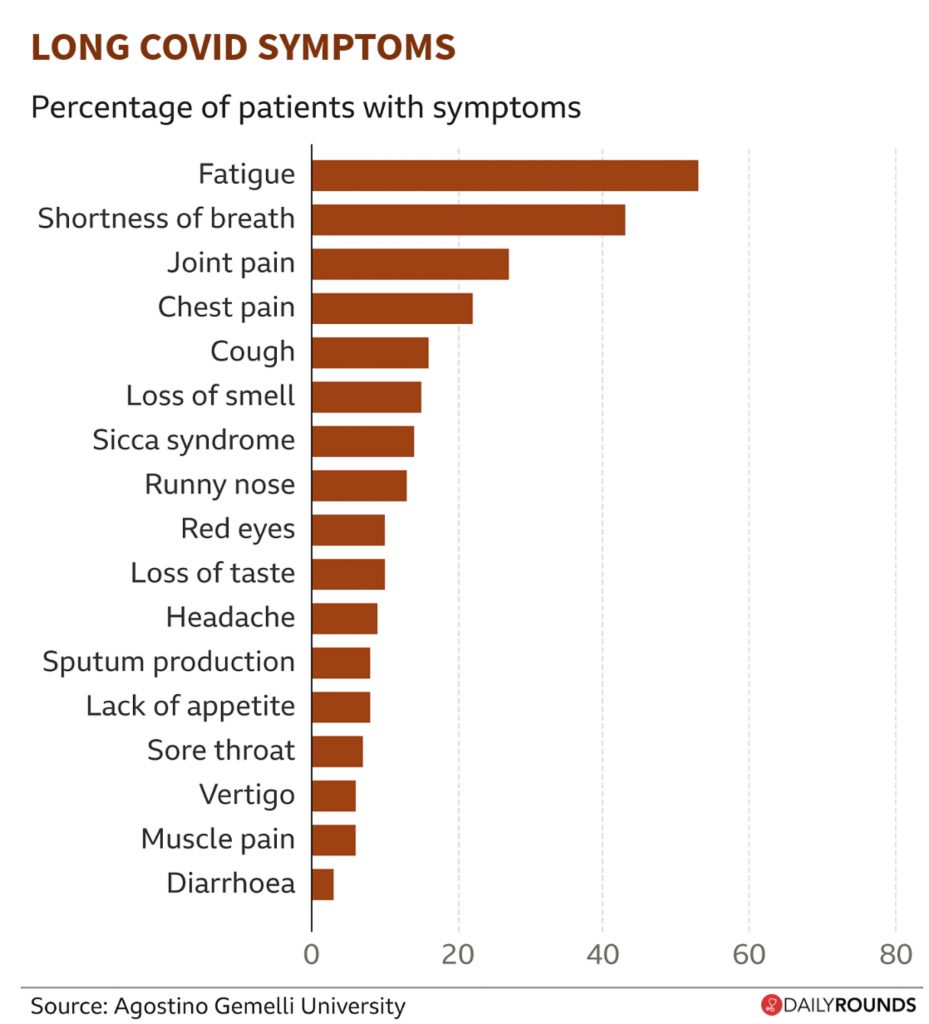
Other symptoms of long COVID include breathlessness, a cough that won’t go away, joint pain, muscle aches, hearing and eyesight problems, headaches, loss of smell and taste as well as damage to the heart, lungs, kidneys, and gut. In addition to this, mental health problems have also been reported including depression, anxiety, and struggling to think clearly.
As we look into it in detail, this long term effects of COVID-19 tend to occur in four main body systems. Which includes, but are not limited to:
Pulmonary:
In most patients. One of the possible long term consequences of COVID-19 is pulmonary fibrosis, which is scarring of the lung tissues. Symptoms of breathlessness may persist, with diminished respiratory muscle strength and abnormalities in lung function tests.
In such cases, it’s a good idea to check the oxygen saturation levels of the patients regularly, especially after exertion. A simple test to perform is a six-minute walk test. In this, you could check the patient’s heart rate and saturation levels at rest, and then after walking for six minutes at the quickest pace he/she can sustain comfortably. The heart rate is expected to rise, but saturation levels should remain steady, above 95 percent.
Cardiac:
One of the long term effects of COVID-19 has been myocarditis, which has been seen in studies of even those patients who had mild or no symptoms. The signs and symptoms include chest pain, fatigue, shortness of breath, and abnormalities of heart rhythm. Patients having irregular heartbeats, commonly referred to as palpitations should be asked to consult the doctor in such cases. An unusually high resting pulse, especially over 100 beats per minute, should also be reported. The good news is that myocarditis is often reversible, but it’s important to keep a close watch.
Neurologic:
One of the common neurological manifestations of long COVID-19 is the loss of smell. This is due to the virus invading the olfactory nerve. Often the loss of smell, accompanied by loss of taste, lasts for several months. Strokes and seizures are rare, but serious complications do occur. Infection with COVID-19 tends to act as a precipitating factor for strokes in those who are already at high risk for it. In addition to this, patients also experience an inability to have a sharp memory or to lack a sharp focus which has been labelled as ‘brain fog’. This clearly affects the day-to-day functioning of an individual.
Mental health:
The COVID-19 has taken a huge toll on mental health across the world, and not just in those who have been Infected. Besides the physical burden of the disease, the stigma that has often been associated with it, and the social isolation has led to a large number of survivors grappling with issues such as anxiety and depression. According to studies, compared with patients who had experienced certain other health events this year — including influenza, kidney stones, or a major bone fracture – those diagnosed with COVID-19 were more likely to have a subsequent psychiatric diagnosis in the following 14 to 90 days.
How many people are affected?
While it remains unclear how many people around the world are affected by long COVID, data from the COVID Symptom Study app suggest that “one in 10 people still have COVID-19 symptoms after 3 weeks.” In addition to this, its latest, unpublished data, suggests as many as one in 50 (2%) of all people infected have long-COVID symptoms even after 90 days.
Similarly, according to a study of 143 people hospitalized with COVID-19 in Italy, 87.4% of patients “reported persistence of at least one symptom, particularly fatigue and dyspnea” two months after discharge from the hospital. However, such studies focus only on the minority of people who end up needing hospital treatment.
As of now, it is unclear as to why certain people are suffering for these long periods; researchers across the globe are currently looking into areas like BMI, age, gender, and ethnicity to see whether these broad factors might give us a better idea of who and why ends up suffering for longer than 30 days.
What needs to be done?
Doctors and experts associated with BMJ recommend that if someone is not recovering from COVID-19: that is if the symptoms aren’t going away or are getting worse even after testing negative for the infection, then consult a doctor immediately.
The doctor should have a clear idea about the post-COVID care being taken by the patient and the duration, intensity, and frequency of symptoms. Specialist investigations and monitoring may be required for patients with long COVID.
Apart from this, people need to understand that long COVID is real and could easily rob them of months (if not years) of their life, and doctors need a clear cut idea and set of guidelines on how to diagnose and monitor people with long-term symptoms. Remember that COVID-19 is a new disease and conditions like long COVID will take some time to be thoroughly studied and have solutions for.
Follow and connect with us on Twitter | Facebook | Instagram