
Breast Milk Donation: How Milk Banks Are Saving Millions Of Infant Lives
Breast milk is indispensable for neonatal care. It plays a crucial role in the overall development and immunity-boosting skills of the newborn. Possibly that’s the reason medical doctors steered that an ailing child admitted in Delhi hospital wanted breast milk despite the fact that they have been feeding the newborn with formula milk.
Born on June 16, the child was just two days old when he was brought to Delhi for treatment of tracheoesophageal fistula with esophageal atresia. The condition, though not uncommon, needs surgical intervention within 48 hours of birth. The lack of facility in their hometown in Leh prompted the family to bring the child to a hospital in Delhi, but the mother couldn’t accompany them due to a C-section delivery and travel restrictions imposed by the COVID-19. The child made a quick recovery soon after the treatment, but the only thing that was missing was the mother’s breast milk. However, since the child wanted breast milk for immunity and swift recovery, bottled breast milk from the mother flew 1000 Kilometres from Leh to Delhi via airplane on a daily basis for over three weeks.
Apart from showing the importance of breast milk this distinctive incident also throws light on the scope of human milk banks, an alternate option for providing infants with mothers milk in such problematic situations. All mothers want to nurse their baby, but unfortunately, some mothers find it challenging to breastfeed their babies either because of low milk production or because of health-related issues. That’s where the Human Milk Bank comes in.
What is a Human Milk Bank?
The human milk bank is a service attached to hospitals or nursing homes where breast milk is collected, screened, and stored from healthy lactating mothers (who willfully donate the milk) to meet the nutritional requirements of babies who are not biologically related to them.
When will it help?
One can consider opting for a donors breast milk in the following situations:
- When the mother experiences low milk production and needs to supplement her own breast milk with the donor’s breast milk.
- If the mother had a double mastectomy and cannot produce breast milk in a sufficient amount.
- If the mother is undergoing treatment with some medications that may interfere with breastfeeding.
- When the mother is suffering from an infectious disease that can pass to the baby through breast milk.
- When someone fosters or adopts babies.
- If the mother had previous surgeries on the breast which affects the milk production.
- If the mother has insufficient glandular tissue and needs supplemental breast milk.
Who can donate?
According to the Human Milk Banking Guidelines published by the Indian Pediatrics, breast milk can be donated by:
- Lactating mothers in good health, good health-related behavior, and not regularly on medications or herbal supplements (with the exception of prenatal vitamins, human insulin, thyroid replacement hormones, nasal sprays, asthma inhalers, topical treatments, eye drops, progestin-only or low dose estrogen birth control products).
- Lactating mothers who are willing to undergo blood testing for screening of infections.
- Mothers having enough milk after feeding their baby satisfactorily.
Who cannot?
Breast milk cannot be donated by:
- Mothers using illegal drugs, tobacco products, or nicotine replacement therapy.
- Mothers regularly taking more than two ounces of alcohol or its equivalent or three caffeinated drinks per day.
- Mother who has a positive blood test result for HIV, HTLV, Hepatitis B or C or syphilis.
- Mother herself or having a sexual partner suffering from HBV, HIV,HCV and venereal diseases.
- Mothers having received an organ or tissue transplant, any blood transfusion/blood product within the prior 12 months.
- Mother who is taking radioactive or other drugs or having chemical environmental exposure or over the counter prescriptions or mega doses of vitamins, which are known to be toxic to the neonate.
- Mother having mastitis or fungal infection of the nipple or areola, active herpes simplex or varicella-zoster infections in the mammary or thoracic region.
Is it safe?
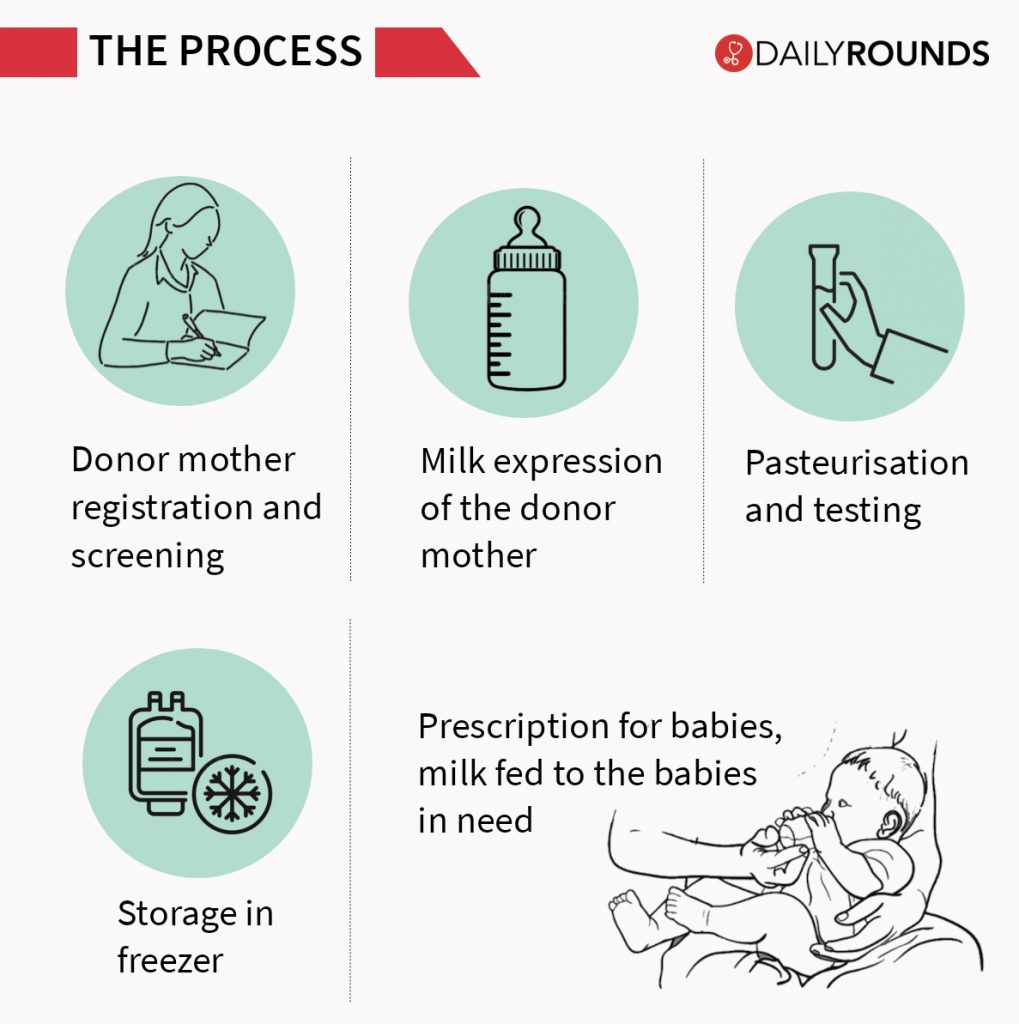
There is a detailed process involved in becoming a breast milk donor and donating milk. The entire process takes about 3-4 weeks and a great deal of care and attention is involved in the process. So there’s nothing much to worry while opting for donated milk from non-profit milk banks.
How does donating help mother and baby?
Donating breast milk helps prevent breast engorgement. Since engorgement makes the breasts firm and swollen, it makes it difficult for the baby to breastfeed properly. Engorgement happens when a mother produces more milk than her baby drinks. In such cases, donating excess milk not only gives relief from pain but also helps save the lives of many needy babies.
Breast Milk Donation In India

Asia’s first human milk donation bank is started nowhere else but in India! The Lokmanya Tilak Hospital, at Mumbai’s Sion, is Asia’s first human milk bank. Nearly 3,000-5,000 babies benefit from its services every year. But the country doesn’t seem to make the most of it even after getting a head start.
Fast forward 30 years from the launch of the first milk bank in the country, India doesn’t have an appropriate number of human milk banks for donating breast milk and to feed its huge number of infants with preterm births. A recent study, landscape analysis of human milk banks in India, reports the gaps of milk banking practices in the country, which need to be addressed for strengthening them. Gaps include sub-optimal financial support from the government, shortage of key human resources, processes and data gaps, and demand-supply gap of donor human milk.
India faces its own unique challenges, having the highest number of low birth weight babies, and significant mortality and morbidity in very low birth weight (VLBW) population. In our country, the burden of low birth weight babies in various hospitals is about 20% with significant mortality and morbidities. Feeding these babies with breast milk can significantly reduce the risk of infections. Hence the Government, health experts and the civil society must join hands to propagate the concept of human milk banking for the sake of thousands of low birth weight and preterm babies.
Given the high infant mortality rate, wherever there is a neonatal intensive care unit, be it district, be it the city, there is an absolute need for a human milk bank with a sufficient number of adequately-sized units to high-quality facilities to encourage mothers to come in and donate their milk.
A Network of Human Milk Banks
At the 11th BRICS summit held recently in Brazil, India along with Russia, China, and South Africa agreed to establish a BRICS Network of human milk banks. This can be seen as an opportune development as the government of India plans to ensure that at least 70% of infants in the country have access to breast milk by the end of 2025.
There is already a similar established network in Europe. The European Milk Bank Association has more than 200 milk banks operating across 20 countries. The impact of such a network could be far-reaching, especially for a developing country like India as it would not only help in saving thousands of newborn lives but also will help the nation to attain sustainable development goals.
Breast Milk Donation During COVID-19
As it is with a lot of services, the pandemic has brought its own set of difficulties in the procurement of donated breast milk as well. However, it has also highlighted the importance of breast milk banks as most of the hospitals in the containment zones separate the newborn from the mother until they test negative for COVID-19 to ensure that the newborns are not infected. During this period, the babies are fed with milk from the human milk bank at the hospitals.
The available data shows that coronavirus does not spread through breast milk. But as a precaution, it is always best for the mother to cover her face with a mask and use gloves while pumping and handling the packets during the donation of breast milk. A recent study published in the Canadian Medical Association Journal (CMAJ) says that pasteurising the donor milk at 62.5 degrees Celsius for 30 minutes inactivates the SARS-CoV-2 virus that causes COVID-19, making it safe for consumption by babies.
There are so many myths surrounding milk banking, donation, and the use of donor breast milk. It was recently that a hospital in Bangladesh suspended its plans to give donated breast milk to needy infants after a backlash by clerics who said that the scheme violated religious laws. Similarly, feeding the infant with milk from another mother is still hard to digest for many people from across the globe. However, they are quite okay in feeding the baby with milk from another species!
Follow and connect with us on Twitter | Facebook | Instagram